Review of Resistance Exercise and Posture Realignment 2001
- Study protocol
- Open Access
- Published:
The effectiveness of a comprehensive corrective exercises program and subsequent detraining on alignment, muscle activation, and motility pattern in men with upper crossed syndrome: protocol for a parallel-grouping randomized controlled trial
Trials volume 21, Article number:255 (2020) Cite this article
Abstruse
Groundwork
Upper crossed syndrome (UCS) refers to specific altered musculus activation and inverse movement patterns along with some postural deviations in the upper quarter of the trunk. This syndrome might contribute to the dysfunction of the cervicothoracic and glenohumeral joints.
Objectives
The nowadays written report will aim to investigate the effectiveness of a comprehensive corrective exercises program (CCEP) and subsequent detraining on alignment, muscle activation and movement pattern in men with UCS.
Methods/pattern
This is a parallel-group randomized controlled trial. Participants will be 22 men anile xviii to 28 years who are suffering from UCS. Participants in the intervention grouping will bear CCEP (3 times a week for eight weeks), followed by 4 weeks of detraining. The command grouping volition do their daily activities. Participants will exist randomized (1:ane) into the intervention or the control group. The primary effect will be upper trapezius activations. Secondary outcomes consist of electromyography of heart and lower trapezius and serratus anterior muscles, scapular dyskinesis test, forward head and shoulder angles, thoracic kyphosis angle, and neck flexion pattern test.
Word
Nosotros propose to evaluate the effectiveness of a randomized controlled trial of a CCEP in men with UCS on their alignment, selected muscle activations, and relevant movement patterns. Results from our trial may provide new insights into the effects of do non only on the alignment but also on muscle activation and movement patterns that are of import outcomes for people with postural malalignments and, if successful, could assist therapists in evidence-based clinical controlling.
Trial registration
Iranian Registry of Clinical Trials, IRCT20181004041232N1. Registered on 26 October 2018.
Background
Most people will see a medical practitioner or another health care provider at least in one case in their lifetime because of neck, shoulder and dorsum pain [1, 2]. At a societal level, these pains are as well responsible for substantial costs, including healthcare expenditure, disability insurance, and work absence [3]. Previous studies showed that these pains might be associated with aberrant alignments [4, 5]. I of these malalignments is the upper crossed syndrome (UCS), which was defined as a muscular imbalance blueprint past Vladimir Janda MD (1923–2002) [vi]. UCS refers to specific altered musculus activation and movement patterns forth with some postural deviations [7]. Alterations in muscle activation include overactivity of the upper trapezius, levator scapula, and pectorals muscles and underactivity of the deep cervical flexors, middle and lower trapezius, and serratus anterior [viii]. Due to kinetic and muscular chains, in that location are altered scapular movement patterns (scapular dyskinesis) and specific postural changes, including forwards caput and shoulder posture and increased thoracic kyphosis [7, 9]. These changes tin can lead to reduction in the stability of the glenohumeral joint and to various musculoskeletal symptoms in the caput, neck, and shoulder [7, 8, ten].
Over recent decades, therapists take been seeking to pattern appropriate exercises to correct musculoskeletal malalignments mainly through structural and functional approaches [11,12,xiii]. In the traditional structural approach, the changes observed in malalignments such equally in UCS are attributed to biomechanics and are presumed to lead to adjustments in the length and force of local muscles [eleven, 14]. This may account for the stretching of brusque muscles and strengthening of weakened muscles at the site of the problem in the correction phase, while ignoring other related malalignments [14]. Interestingly, despite the popularity of this method, very little research has been conducted based on this theory [15]. Furthermore, some review studies have questioned the effectiveness of strengthening and stretching exercises to improve postural disorders [16, 17].
In contrast, the functional (neurological) approach to musculoskeletal problems is based on the interaction of the central and peripheral nervous systems, and the involvement of the muscular and skeletal structures in producing and controlling motility [six, 18, nineteen]. In this functional arroyo, the musculoskeletal problems are attributed to the function of muscles in motor function; furthermore, changes in the alignment outcome not only from changes in muscle length and strength but also from more important changes in musculus neuromuscular factors, such as muscle recruitments [13, twenty]. In fact, the motor control unit may change the muscle activation strategy for temporary stabilization due to the presence of dysfunction. These changes in motor recruitment will change the muscular balance, move patterns, and somewhen the motor program [12]. Similarly, Hodges et al. noted that motor command interventions require tailoring to each individual's posture, muscle activation, and movement pattern [21]. However, this theory has not been tested in practice for the prevention and treatment of musculoskeletal malalignments.
Hence, for the assessment of UCS, the alignment and its side furnishings are frequently evaluated, such as increment in thoracic kyphosis or forward head angles, while less attending has been paid to the keystone, i.e., the scapulae, and the relevant altered muscle activation and movement patterns [22]. In this regard, many researchers and therapists have but evaluated one of the affected regions, such as caput, shoulders, or spine, separately and reported a caste of postural departure regardless of other relevant malalignments and patterns of the muscle activation and related motion patterns, such as scapulohumeral rhythm or neck flexion [23,24,25]. In add-on, the design and implementation of the training protocol are based on the traditional structural approach, in which stretching exercises for short muscles and strengthening exercises for weak muscles are prescribed at the site of malalignment [22, 24], while the neuromuscular factors and related motility patterns may not be considered. To the best of our knowledge, no studies identifying and correcting UCS have considered the iii components of alignment, movement blueprint, and muscle activity in both assessment and correction processes.
Study objectives
The primary aim of the present study is to evaluate the effectiveness of a comprehensive cosmetic exercise plan (CCEP) in young men with UCS for 8 weeks, every bit measured by alignment (position of the scapula, head and cervix, shoulder, and thoracic spine), electromyography activeness of selected muscles (upper, middle and lower trapezius, serratus anterior), and specific move patterns (scapulohumeral rhythm and cervix flexion). A secondary aim is to evaluate the effects of the plan later 4 weeks of detraining after the intervention.
Methods/pattern
Study design
This is a parallel-group randomized controlled trial comparing an intervention grouping receiving an eight-week CCEP followed by four weeks of detraining to a control group who volition but do their daily activities. The study will be performed at the Laboratory of Wellness and Sports Medicine Department, University of Tehran, Tehran, Iran. Initially, participants will take part in the baseline assessment procedure. They will then receive the intervention for eight weeks. Subsequently the stop of the intervention stage, all the measurements volition be repeated. Finally, a follow-upwards assessment will be performed subsequently a 4-week detraining period. The study schedule is presented in Tabular array i and a flow diagram is shown in Fig. ane. The study protocol is reported in accordance with the SPIRIT guideline.
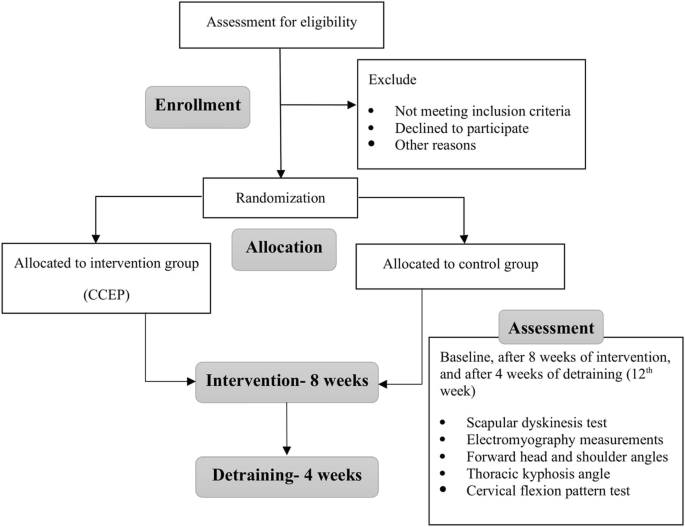
Study flowchart
Ethical aspects
Before starting the projection, all participants will be asked to complete and sign an informed consent form. Ethics approval was obtained on August 28, 2017, from the Ideals Commission on Enquiry at University of Tehran, Iran (IR.UT.REC.1395026). The protocol was approved at the Iranian Registry of Clinical Trials on 2018-10-26 (IRCT20181004041232N1).
Study participants and eligibility criteria
The participants consist of 24 men with UCS aged eighteen to 28 years. They will exist recruited from the students of the University of Tehran, Iran, through advertisements on bulletin boards. They will be screened primarily past observation for 3 main factors related to UCS, including altered alignment, muscle activation, and movement patterns. Since the scapulae are the keystone in UCS, participants who have any abnormality in the position and rhythm of the scapula, as measured by the scapular dyskinesis exam, will exist recruited. In addition, they will be assessed for presenting any postural changes such as forward head (≥ 44°), round shoulder (≥ 49°), or excessive thoracic kyphosis (≥ 42°) as measured by photogrammetry and flexicurve, respectively [15]. Also, to ensure whatsoever change in musculus activation is related to postural changes, some confirmatory tests, including muscle length tests for upper trapezius and pectoral muscles besides every bit musculus force tests for eye and lower trapezius and deep cervical flexor, will be used. Individuals will exist excluded from the research process if they do actress physical activeness and sports that may touch on the outcomes of the research, have any visible malalignment in the pelvis and lower extremities, take a history of fracture, surgery, or joint diseases in the spine, shoulder and pelvis, take a rotation greater than 5° on the frontwards bending test because of scoliosis [fifteen], or take a bodyweight outside the normal range (torso mass index betwixt 18 and 25) [23].
Randomization
Participants will exist randomized using calculator-generated block randomization in a 1:1 ratio, followed by a curtained resource allotment through opening sequentially numbered, opaque and sealed envelopes; a menu inside will indicate the group into which the participant will randomly be allocated, i.e., the intervention or the command grouping. Participants can discontinue the projection at whatever fourth dimension. However, all efforts will exist fabricated to avoid missing data. The specific way to deal with missing data will be determined at a information review coming together before starting statistical analyses.
Comprehensive approach
The comprehensive arroyo (Fig. 2), which is a new approach to corrective exercises [xv], takes advantage of the strengths and weaknesses of traditional approaches to achieve the best outcome in correcting musculoskeletal malalignments. It was initiated in 2014 by Seidi et al., who compared the efficacy of comprehensive and traditional corrective exercise programs on the kyphosis bending [15]. The full general purpose of this arroyo is to pay attending to alignment, muscle activation, and move design simultaneously beyond the whole body rather than at just a single site during both the cess and correction phases.
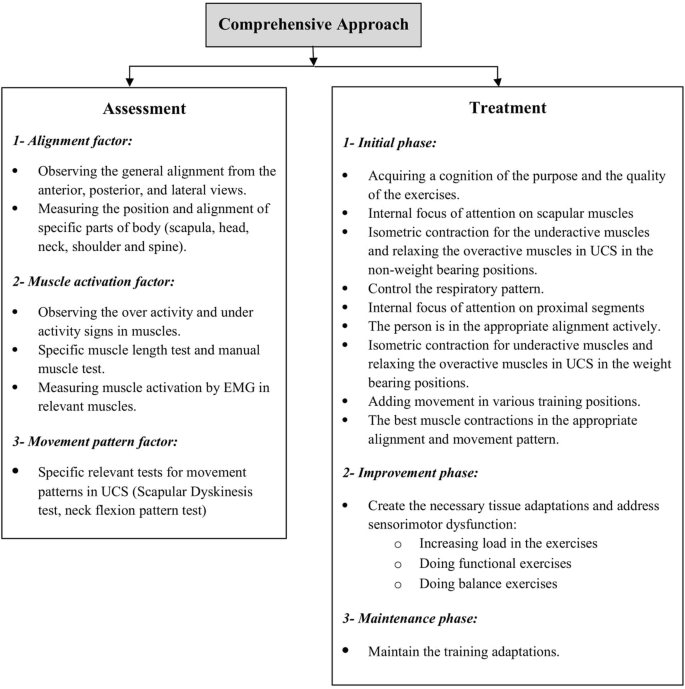
Comprehensive approach flowchart
Intervention
An 8-week CCEP volition be structured to include three phases. In the initial stage of the exercise program, the participants will become cognizant of the purpose and the quality of the exercises. This is characterized as voluntary command of exercise, requiring cortical regulation of movement and a lot of concentration on the part of the participants [12]. Participants will be asked to focus simply on the scapular muscles, i.e., an internal focus [26] while their alignment is corrected passively. So, the exercises volition be executed in non-weight bearing positions and the participants only try to contract underactive muscles isometrically and relax overactive muscles around the scapula for normalization of scapular position and motion [27, 28]. The participants will be instructed to reproduce this orientation of scapula actively using auditory (from therapist) and kinesthetic cues such equally palpation [28]. Once a participant regains sufficient command over scapular muscles, he volition focus externally on it and plough the internal focus of attention to correcting proximal segments through chin tuck, retraction of shoulders, and straightening the upper thoracic spine [29]. Then, he volition do the exercises in dissimilar weight-bearing positions, and after restoring muscle balance in the static conditions, he will try to add upper extremity movements in various grooming positions. Also, the respiratory design of participants will be controlled during this phase and necessary feedback will be provided [13]. Since the quality of exercises is highly important in this phase, the participants should not feel drawn while doing the exercises because fatigue may alter optimal muscle activations and move patterns [thirty].
Once the participants can contract the appropriate muscles in a correct alignment during the best movement pattern, they should be able to maintain this for a long time. This goal will be addressed in the improvement stage when necessary tissue adaptations occur by increasing the load of exercises [31, 32]. Placing the participants in weight-bearing positions and using some tools such as grooming balls and Thera-Bands will reinforce their abilities gradually. During this phase, the participants will just focus on the goal of exercises (external focus) [29]. Moreover, because UCS is representative of underlying potential sensorimotor dysfunction, some functional balance exercises volition be included [12]. The frequency and intensity of the exercises will increase progressively during the study, provided that participants can demonstrate good-quality movement. In the final phase, i.eastward., the maintenance phase, the participants will try to maintain the training adaptations [32]. All exercises will be performed under the supervision of a cosmetic do specialist. The participants will not comport any extra exercises at domicile. However, they will exist asked to avoid sustaining poor posture. More than details about the intervention protocol are presented in Appendix 1. The control group volition exist asked to do their ordinary daily activities and not to participate in any exercise programs. After the report is completed, the control group will undergo the exercise intervention protocol for ethical reasons.
Event measures
All outcome measurements will exist performed by the main researcher at baseline, eight weeks (after intervention), and 12 weeks (follow-up). Demographic information (i.due east., sex, age, body mass alphabetize) will be measured before the intervention.
Outcome measures
Upper trapezius activation (measured with surface electromyography) is the primary effect measure. Secondary outcomes include electromyography measurements of heart and lower trapezius and serratus anterior muscles, scapular dyskinesis, forwards head and shoulder angles, thoracic kyphosis bending, and cervix flexion pattern.
Electromyography measurements
Surface electromyography of the scapular stabilizer muscles (including upper, eye, lower trapezius, and serratus anterior) will be performed using an ME-6000 Megawin. The participants will execute humeral abduction without resistance in three phases (concentric, isometric, and eccentric) lasting for 3 s each. They will already accept been trained to move correctly and at the correct speed so that they can perform the movement five times; residuum time is three southward betwixt movements. Disposable Ag-AgCl electrodes with a bore of 2 cm and a 2 cm spacing between two poles of electrodes will be used and information will be recorded at a frequency of k Hz. The location of the electrodes volition be adamant using the SENIAM protocol and based on valid scientific papers [33, 34]. The maximum voluntary isometric wrinkle (MVIC) will be recorded to normalize the signals. More details most the location of the electrodes and MVIC positions are presented in Appendix ii. The data from the mean foursquare root (RMS) will exist used in the procedure of measuring musculus activation. To determine the onset of muscle activity, just the concentric phase of the motility volition be used and information technology will exist based on the onset of the deltoid muscle. Moreover, the onset of the activity will be from the indicate where the level of muscle activeness reaches ii standard deviations higher up the rest of the muscle activity [34].
Scapular dyskinesis
The current recommendation for clinical assessment based on a prior consensus meeting is the employ of the dynamic scapular dyskinesis examination according to the process described by McClure et al. [35]. The position and move of scapula are characterized by dyskinesis as a "yes" (presence of deviation or dysrhythmia/asymmetry bilaterally) or "no" (no presence). This method has been shown to be reliable amongst observers and has acceptable clinical utility [35, 36].
Forward head and shoulder angles
The angle of the caput and the shoulder will be measured using photogrammetry according to the process described by Seidi et al. [15]. The validity and reliability of this method take been established in previous studies [37, 38].
Thoracic kyphosis bending
To mensurate the static alignment of the thoracic spine, the flexicurve method volition exist used, which is a well-established, valid, and reliable technique [39, forty]. A detailed clarification of the procedure tin exist establish in previous studies [xv, 23].
Neck flexion design exam
The participants will lie supine with knees bent. They volition then be instructed to lift the head and look at their toes. Normal motility produces a smooth reversal of the normal cervical lordosis, keeping the mentum tucked. Abnormal movement is compensated by the tightness of the SCM, producing an early protraction of the chin directly upward at the kickoff of the motion [8].
Sample size
The sample size was calculated using the 1000*Power software (Chiliad*Power, version 3.0.10, Frg). It was based on a airplane pilot test of seven participants, and on the assumption that a x% difference in musculus activity [34] and an 11° departure in kyphosis angle [41] between groups would institute clinically meaningful differences. Information technology was calculated that a sample consisting of at least 18 participants would suffice to obtain 80% power with d = 0.80 result size, and a confidence interval of 0.95. Information technology should be noted that the issue size was reported in the previous study which compared scapular musculus activity betwixt the interventions and control groups. Effect sizes ranged from 0.half-dozen to 0.9 for the EMG amplitude and onset [42]. Since a few participants may drop out of the intervention studies, we will include 24 (assuming a drop-out rate of approximately 25%).
Statistical method and assay
Assessments of statistical procedures volition exist performed using IBM SPSS version xx for Windows (SPSS Inc., Chicago, IL, USA). All variables volition be reported using the descriptive statistic (mean, standard difference). Shapiro-Wilk test will be used to assess the normality of data. Repeated measures ANOVA will be used to compare the means. If mean deviation is significant, then the Bonferroni-adjusted post-hoc exam will be calculated. The independent t-test will as well be used for comparison between groups. Finally, the effect size will be calculated for the magnitude of the difference using the Cohen method. The significance level will be set up at p < 0.05.
Discussion
We advise to evaluate the effectiveness of a randomized controlled trial of a CCEP in a group of men aged xviii to 28 years with UCS in terms of their alignment, selected muscle activation, and relevant movement patterns.
Clinicians believe that it is important to quantify caput, shoulder, scapulae, and spinal posture beliefs as they influence and are influenced by many biomechanical, motor control, and performance variables [43]. It has been causeless that exercise can correct postural malalignment, but an before review found piffling evidence to support this assumption [17]. Moreover, despite the widespread inclusion of postural correction in do interventions, there are limited empirical data to back up its effectiveness and little is known about the near effective practise interventions [24]. As already mentioned, information technology seems the well-nigh important reason is the adherence to the traditional structural arroyo in the previous studies. We want to bear a randomized controlled trial based on the comprehensive arroyo which is fairly powered and utilizes validated result measurements of UCS to investigate the effects of the CCEP on both our primary and secondary outcomes. If the CCEP results in irresolute the alignment, muscle activation, and motion design, or all three, nosotros will examine the pathways of modify to make up one's mind whether changes in the alignment, muscle activation, or move pattern can account for the change in the UCS symptoms. Furthermore, if we find out that the CCEP tin meliorate a postural malalignment like in UCS, this evidence could enable practitioners to recommend early intervention for UCS to forbid or delay UCS-associated consequences. Therefore, various experts in the field of corrective exercises and physical therapy, equipped with the knowledge on these changes, can identify people with UCS and also adopt advisable therapeutic strategies to correct it and forbid the occurrence of secondary consequences.
Our study has some limitations including the recruitment of just men eighteen to 28 years of age. Therefore, the results of this written report will not be generalizable to all people (e.g., women or men aged ≥ 28 years) with UCS. Another limitation is that this written report is not a double-blind pattern since it is not possible, every bit is the example with most exercise trials.
The results of our written report will be presented at scientific conferences and published in bookish journals to ensure that our study will inform therapists in practice and prove benign to patient care. Our goal is to conduct a clinical trial that will provide therapists with bear witness of the efficacy of the CCEP on the keystone and the side effects of UCS. Previous trials take often used only cess of the alignment to investigate the comeback of a malalignment. Withal, we are focusing on alignment, muscle activation, and movement pattern simultaneously based on the comprehensive approach. Therefore, if our do intervention proves successful, our approach to improving UCS could stand for a fundamental epitome shift in exercise intervention strategies to ameliorate postural malalignments and their consequences. Results from our trial may provide new insights into the furnishings of practise non only on alignment only as well on muscle activation and motion pattern, which are important outcomes for people with postural malalignments and, if successful, information technology could assist practitioners in individualized clinical decision-making. However, our results may have a limited transferability to all people and thus may exist valid only for men.
Trial status
This trial was registered on 2018-10-26 (registration number IRCT20181004041232N1, protocol version number 34266, https://en.irct.ir/user/trial/34266/view). The trial is currently in the stage of recruiting patients. The first patient was included on 2019-02-01. To date, ten patients have been included. The recruitment volition be completed on approximately 2019-07-01.
Availability of information and materials
The authors aim to make the datasets supporting the results and conclusions of this study bachelor as supplementary files in future published articles.
References
-
Langenfeld A, Humphreys BK, de Bie RA, Swanenburg J. Upshot of manual versus mechanically assisted manipulations of the thoracic spine in neck pain patients: written report protocol of a randomized controlled trial. Trials. 2015;16(ane):233.
-
Gaffney BM, Maluf KS, Davidson BS. Evaluation of novel EMG biofeedback for postural correction during computer utilize. Appl Psychophysiol Biofeedback. 2016;41(2):181–9.
-
Kamper SJ, Apeldoorn A, Chiarotto A, Smeets R, Ostelo R, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back hurting: Cochrane systematic review and meta-analysis. BMJ. 2015;350:h444.
-
Yoo West-G, Park Due south-Y. Furnishings of posture-related auditory cueing (PAC) program on muscles activities and kinematics of the neck and torso during calculator work. Work. 2015;50(ii):187–91.
-
Barrett E, O'Keeffe K, O'Sullivan K, Lewis J, McCreesh K. Is thoracic spine posture associated with shoulder pain, range of movement and office? A systematic review. Man Ther. 2016;26:38–46.
-
Morris CE, Greenman PE, Bullock MI, Basmajian JV, Kobesova A. Vladimir Janda, Medico, DSc: tribute to a master of rehabilitation. Spine. 2006;31(nine):1060–four.
-
Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6(1):51.
-
Page P. Cervicogenic headaches: an show-led arroyo to clinical management. Int J Sports Phys Ther. 2011;6(3):254.
-
Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44(5):300–5.
-
Kang J-H, Park R-Y, Lee S-J, Kim J-Y, Yoon S-R, Jung K-I. The effect of the forwards head posture on postural balance in long time computer based worker. Ann Rehabil Med. 2012;36(ane):98–104.
-
Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal airplane. Scoliosis Spinal Disord. 2018;13(1):6.
-
Page P. Sensorimotor preparation: a "global" approach for balance training. J Bodyw Mov Ther. 2006;ten(i):77–84.
-
Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization & sports rehabilitation. Int J Sports Phys Ther. 2013;8(1):62.
-
Sahrmann S, Azevedo DC, Van Dillen L. Diagnosis and treatment of motility system harm syndromes. Braz J Phys Ther. 2017;21(6):391–9.
-
Seidi F, Rajabi R, Ebrahimi I, Alizadeh MH, Minoonejad H. The efficiency of cosmetic practise interventions on thoracic hyper-kyphosis angle. J Dorsum Musculoskelet Rehabil. 2014;27(i):seven–16.
-
Hrysomallis C. Effectiveness of strengthening and stretching exercises for the postural correction of abducted scapulae: a review. J Strength Cond Res. 2010;24(2):567–74.
-
Hrysomallis C, Goodman C. A review of resistance do and posture realignment. J Force Cond Res. 2001;15(3):385–90.
-
Hamill J, van Emmerik RE, Heiderscheit BC, Li 50. A dynamical systems approach to lower extremity running injuries. Clin Biomech. 1999;14(v):297–308.
-
Davids 1000, Glazier P, Araujo D, Bartlett R. Motion systems as dynamical systems. Sports Med. 2003;33(4):245–60.
-
Janda Five. On the concept of postural muscles and posture in man. Aust J Physiother. 1983;29(3):83–4.
-
Hodges P, Paul Due west, Van Dieën JH, Cholewicki J. Fourth dimension to reflect on the part of motor control in low dorsum hurting. Alexandria: JOSPT Inc.; 2019.
-
Bae WS, Lee HO, Shin JW, Lee KC. The result of center and lower trapezius strength exercises and levator scapulae and upper trapezius stretching exercises in upper crossed syndrome. J Phys Ther Sci. 2016;28(five):1636–9.
-
Vaughn DW, Brownish EW. The influence of an in-abode based therapeutic exercise plan on thoracic kyphosis angles. J Back Musculoskelet Rehabil. 2007;twenty(4):155–65.
-
Harman One thousand, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve frontwards head posture in normal adults: a randomized, controlled x-week trial. J Man Manipulative Ther. 2005;thirteen(3):163–76.
-
Hajihosseini E, Norasteh A, Shamsi A, Daneshmandi H. The effects of strengthening, stretching and comprehensive exercises on frontwards shoulder posture correction. Phys Treat Specif Phys Ther J. 2014;4(three):123–32.
-
Cools AM, Struyf F, De Mey M, Maenhout A, Castelein B, Cagnie B. Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br J Sports Med. 2013. https://doi.org/x.1136/bjsports-2013-092148.
-
Kibler WB, Sciascia AD, Uhl TL, Tambay Northward, Cunningham T. Electromyographic analysis of specific exercises for scapular command in early phases of shoulder rehabilitation. Am J Sports Med. 2008;36(9):1789–98.
-
Worsley P, Warner M, Mottram S, Gadola S, Veeger H, Hermens H, et al. Motor control retraining exercises for shoulder impingement: furnishings on function, muscle activation, and biomechanics in young adults. J Shoulder Elb Surg. 2013;22(4):e11–e9.
-
Lederman E. The myth of cadre stability. J Bodyw Mov Ther. 2010;14(ane):84–98.
-
Tsai N-T, McClure Prisoner of war, Karduna AR. Effects of muscle fatigue on 3-dimensional scapular kinematics1. Curvation Phys Med Rehabil. 2003;84(7):1000–5.
-
Brody LT. Constructive therapeutic exercise prescription: the right exercise at the right dose. J Paw Ther. 2012;25(2):220–32.
-
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee I-Yard, et al. American College of Sports Medicine position stand up. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59.
-
Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361–74.
-
De Mey Thousand, Danneels L, Cagnie B, Cools AM. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms result of a vi-calendar week training program on muscle recruitment and functional issue. Am J Sports Med. 2012;40(8):1906–xv.
-
McClure P, Tate AR, Kareha Due south, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160–four.
-
Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia Advert. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the 'Scapular Summit'. Br J Sports Med. 2013;47(14):877–85.
-
Gadotti IC, Armijo-Olivo S, Silveira A, Magee D. Reliability of the craniocervical posture assessment: visual and angular measurements using photographs and radiographs. J Manip Physiol Ther. 2013;36(9):619–25.
-
Ruivo RM, Pezarat-Correia P, Carita AI. Intrarater and interrater reliability of photographic measurement of upper-body continuing posture of adolescents. J Manip Physiol Ther. 2015;38(1):74–fourscore.
-
Greendale One thousand, Nili N, Huang M-H, Seeger Fifty, Karlamangla A. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the continuing radiological Cobb angle. Osteoporos Int. 2011;22(vi):1897–905.
-
Barrett East, McCreesh M, Lewis J. Reliability and validity of not-radiographic methods of thoracic kyphosis measurement: a systematic review. Man Ther. 2014;nineteen(1):10–7.
-
Carman D, Browne R, Birch J. Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J Bone Joint Surg Am. 1990;72(three):328–33.
-
Derakhshani A, Letafatkar A, Khosrokiani Z. Comparison the effects of SUREE programs on people with scapular downwardly rotation syndrome: a randomized clinical trial. J Sport Rehabil. 2018;28(8):787–95.
-
Claus AP, Hides JA, Moseley GL, Hodges PW. Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements. Appl Ergon. 2016;53:161–8.
Acknowledgments
We are thankful to the participants for their participation. Nosotros besides admit the defended inquiry professionals who contribute to the intervention and cess of the participants in this written report.
Dissemination
The written report results will be published in peer-reviewed journals.
Funding
The authors state no external or internal funding involved.
Author data
Affiliations
Contributions
MBT and FS designed the trial. MBT, FS, and HM participated in trial registration, evaluation, and monitoring. MBT performed the exercises. LLA and PP have contributed to drafting the manuscript and revising it critically for important intellectual content. MBT, HM, LLA, and PP participated in the pattern of the statistical analysis. All authors contributed to the refinement of the study protocol and approved the terminal manuscript.
Corresponding author
Ethics declarations
Ideals approval and consent to participate
Ethics approving was obtained on August 28, 2017, from the Ethics Committee on Enquiry in Academy of Tehran, Iran (IR.UT.REC.1395026). Before starting the projection, all participants volition exist asked to complete the written consent class.
Consent for publication
Written informed consent was obtained from the person for publication of his accompanying images in this manuscript.
Competing interests
The authors declare that they take no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Comprehensive corrective exercise program
The elapsing of the exercise protocol is eight weeks, with three sessions per calendar week, and each session volition be about an 60 minutes. Each exercise session begins with 10 min of warm-up activity and ends with 5 min of cool-downwardly. Selected exercises are designed in three phases: initial, improvement, and maintenance [35].
Initial phase exercises
The initial phase exercises (Fig. 3) include laying supine on a foam coil in three different arm abduction angles (exercise 1A–C), side-lying external rotation (do ii), side-lying forrard flexion (practice 3), standing diagonal flexion (exercise 4), and military press (exercise 5). Participants with less ability can practise exercises 4 and 5 in a sitting position. Once a participant regains muscle residuum in the static atmospheric condition, he will endeavor to add upper extremity movements in exercise positions. Exercises progress in frequency and intensity during this stage, every bit long every bit participants are able to demonstrate proficient quality move. The initial phase elapsing is 2 weeks and the exercises will be performed for seven sets of 10-s hold to ten sets of 15-s hold.
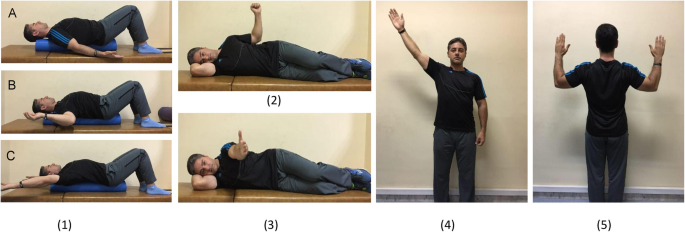
The initial phase exercises
Improvement phase exercises
The goal of the improvement phase is to create the necessary tissue adaptations in the participant. Therefore, during this phase Thera-Bands, weights, and grooming balls will be used. Improvement phase exercises (Fig. 4) include side-lying external rotation with a dumbbell (exercise 6), side-lying forward flexion with a dumbbell (practise 7), standing diagonal flexion with a dumbbell (exercise eight), continuing external rotation with Thera-band (do 9), standing diagonal flexion with Thera-band (exercise ten), abduction in sitting on a preparation ball (exercise 11), lying prone V, T, and W exercises (exercise 12), and abduction in standing on a balance board (practise xiii). Exercises are progressed by considering individual characteristics of each participant and by observing the overload principle and the progression in the number of repetitions of each prepare during the 4 weeks of the comeback phase. The exercises will be performed from five sets of x repetitions to six sets of xv repetitions.
Maintenance stage exercises: The exercises are the aforementioned as in the improvement stage without any progression in intensity and frequency. The maintenance phase elapsing is ii weeks.

The improvement phase exercises
Appendix 2
Rights and permissions
Open Access This article is distributed under the terms of the Artistic Commons Attribution iv.0 International License (http://creativecommons.org/licenses/by/iv.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you requite advisable credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Eatables Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the information made available in this article, unless otherwise stated.
Reprints and Permissions
Most this article
Cite this article
Bayattork, M., Seidi, F., Minoonejad, H. et al. The effectiveness of a comprehensive cosmetic exercises program and subsequent detraining on alignment, muscle activation, and movement pattern in men with upper crossed syndrome: protocol for a parallel-group randomized controlled trial. Trials 21, 255 (2020). https://doi.org/x.1186/s13063-020-4159-9
-
Received:
-
Accustomed:
-
Published:
-
DOI : https://doi.org/10.1186/s13063-020-4159-nine
Keywords
- Corrective exercises
- Alignment
- Muscle activation
- Motion pattern
- UCS
Source: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-4159-9
0 Response to "Review of Resistance Exercise and Posture Realignment 2001"
Post a Comment